HIP
1. Arthritis
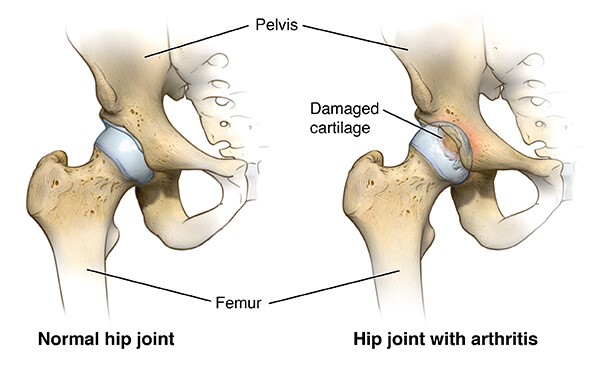
Hip arthritis commonly describes the most common form of hip arthritis, which is known medically
as hip osteoarthritis.
Hip osteoarthritis is a joint disease that mostly affects your hip joint cartilage. Articular cartilage
is the hard slippery surface that covers the sections of bones that move against each other in your hip
joint.
Healthy articular cartilage allows your hip joint bones to smoothly and painlessly glide over each other
and also helps to absorb any shock forces not dispersed by your hip muscles.
Symptoms of Hip Arthritis?
Hip arthritis results in hip pain, joint weakness, joint instability, and restrictions of movement that interfere with your most basic daily tasks such as walking, climbing stairs or driving.
Your symptoms can develop suddenly or slowly and may include:
2. AVN avascular necrosis
Avascular necrosis is the death of bone tissue due to a lack of blood supply. Also called osteonecrosis,
it can lead to tiny breaks in the bone and the bone’s eventual collapse.
A broken bone or dislocated joint can interrupt the blood flow to a section of bone. Avascular necrosis
is also associated with long-term use of high-dose steroid medications and excessive alcohol intake.
Anyone can be affected, but the condition is most common in people between the ages of 30 and 50.
Symptoms
Many people have no symptoms in the early stages of avascular necrosis. As the condition worsens, your
affected joint might hurt only when you put weight on it. Eventually, you might feel the pain even when
you’re lying down.
Pain can be mild or severe and usually develops gradually. Pain associated with avascular necrosis of
the hip might centre on the groin, thigh or buttock. Besides the hip, the areas likely to be affected
are the shoulder, knee, hand and foot.
Some people develop avascular necrosis on both sides (bilaterally) — such as in both hips or in both
knees.
What are the Causes:
Avascular necrosis occurs when blood flow to a bone is interrupted or reduced. Reduced blood supply can be caused by:
Risk factors
Risk factors for developing avascular necrosis include:
Complications
Untreated, avascular necrosis worsens with time. Eventually, the bone can collapse. Avascular necrosis also causes bone to lose its smooth shape, potentially leading to severe arthritis.
Prevention
To reduce your risk of avascular necrosis and improve your general health:
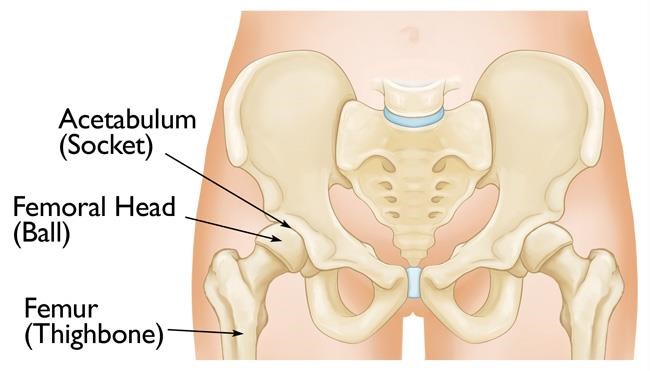
3. Acetabulum Reconstruction
Fractures of the acetabulum are challenging orthopaedic injuries to repair, at times leaving multiple
small fragments of fractured bone and cartilage. Compounded by the location in a region challenging in
which to work and fraught with risk, these “puzzle pieces” must be brought back together to restore hip
function and mobility.
The acetabulum, commonly thought of as the socket of the ball-and-socket hip joint, may break in one of
10 different pattern.
Relative to hip fracture, acetabular fracture is uncommon. These fractures occur in two distinct patient
populations:
Patients’ pain levels vary widely and are related to the injury pattern and mechanism of injury.
Risks with acetabular fracture
This fracture puts patients at considerable risk of developing post-traumatic arthritis, which may result
in the need for hip replacement. Post-traumatic arthritis occurs due to damage to the articular surface
of either the acetabulum or femoral head. Another potential complication with acetabular fracture is
avascular necrosis, in which the blood supply to the femoral head is sufficiently damaged or stretched
from dislocation that the bone subsequently dies and collapses, resulting in hip pain.
Acetabular fractures are commonly associated with multiple other injuries, such as to the abdomen, chest
or head. With isolated acetabular fracture, the risk of shock is low, but concomitant injuries must be
identified and treated appropriately.
Surgical treatment of acetabular fracture is complex and can result in complications and poor outcomes.
While the infection risk is similar to that of other hip procedures, body mass index (BMI) is a
predictor of infection and complications of operative treatment.
Fracture management
When patients with suspected acetabular fracture arrive at any hospital, the first order of business is
to determine if the hip is reduced or dislocated. If dislocated, providers should perform urgent closed
reduction prior to any transfers, as this procedure is crucial to preventing future complications.
If the hip is unable to be reduced or appears widely displaced, consult with a higher level trauma
centre for transfer.
Physical exams for patients who have potentially suffered this injury are minimal, usually
differentiating between acetabular or hip fracture.
4. Total HIP replacement
Hip replacement (total hip arthroplasty) is surgery to replace a worn out or damaged hip joint. The
surgeon replaces the old joint with an artificial joint (prosthesis). This surgery may be a choice after
a hip fracture or for severe pain because of arthritis.
Various types of arthritis may affect the hip joint:
The goal of hip replacement surgery is to replace the parts of the hip joint that have been damaged. It
also helps relieve hip pain that can’t be controlled by other treatments.
A traditional hip replacement involves an incision several inches long over the hip joint. A newer
approach uses 1 or 2 smaller incisions to do the surgery. This is called minimally invasive hip
replacement. But the minimally invasive procedure is not suited for all people who need hip replacement.
Your healthcare provider will figure out the best procedure for you.
When do I require hip replacement surgery?
Hip replacement surgery is a treatment for pain and disability in the hip. Osteoarthritis is the most
common reason for hip replacement surgery.
Osteoarthritis causes loss of joint cartilage in the hip. Damage to the cartilage and bones limits
movement and may cause pain. People with severe pain from degenerative joint disease may not be able to
do normal activities that involve bending at the hip. These activities include walking and sitting.
Other forms of arthritis such as rheumatoid arthritis and arthritis that results from a hip injury can
also damage the hip joint.
Hip replacement may also be used to treat certain hip fractures. A fracture is an injury often from a
fall. Pain from a fracture is severe. Walking or even moving the leg causes pain. Your healthcare
provider may have other reasons to recommend a hip replacement surgery.
5. Revision HIP replacement
When a replacement joint wears out, loosens or develops a problem, it can be resurfaced or replaced in a
joint revision operation. Using regular X-ray examinations, the orthopaedic surgeon can detect and
monitor any changes, and plan for revision surgery before a major problem develops.
Revision hip surgery requires the removal of the previous prosthesis, the cement, the surrounding tissue
and the dead bone before a new prosthesis can be inserted.
Postoperative care for revision hip surgery is the same as that for total hip replacement surgery.
Patients receive a combination of home healthcare, physical and occupational therapy home health care
and other forms of rehabilitation.
Complications from this procedure, in addition to the risks associated with any major surgery, are
similar to those for original joint replacement surgery. However, the success rate for revision surgery
is usually lower than that for the original surgery because the bone is weaker.